Mpox
Update September 2024
Mpox, formerly referred to as ‘Monkeypox’, is caused by a virus that belongs to the Orthopoxvirus family, the same group as the smallpox virus. It is usually present in some countries in Central and West Africa (“endemic countries”).
On 14 August 2024 the World Health Organization (WHO) declared mpox virus a Public Health Emergency of International Concern (PHEIC).
A PHEIC is defined by the International Health Regulations (IHR) of the WHO as, “an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response”. This definition implies a situation that is serious, sudden, unusual or unexpected; carries implications for public health beyond the affected State’s national border; and may require immediate international action.
This PHEIC determination is the second in two years relating to mpox. In July 2022, a multi-country outbreak of mpox was declared a PHEIC as it spread rapidly across a range of countries where the virus had not been seen before. That PHEIC was declared over in May 2023 after there had been a sustained decline in global cases.
CERN is monitoring the situation closely. At the present time, no CERN specific recommendations apply.
Below you will find some further information and general advice about mpox.
Transmission
Animal to human transmission can occur through contact with an infected animal, from an animal bite, or contact with its blood or other bodily fluids. Infection can also occur if a person touches the rash on an infected animal's skin - which sometimes happens during food preparation. In endemic countries, the mpox virus is found among rodents and non-human primates, but it is assumed that any mammal can catch the disease.
Prior to the outbreak in 2022, human to human transmission was uncommon, however this is now changing.
Transmission between humans occurs mainly via direct contact with skin and mucous membranes, as well as contact with infected secretions from skin and mucous membrane vesicles or sores, particularly during sexual intercourse.
Nonetheless, other routes for transmission may occur.
The virus can also be transmitted via infected scabs, respiratory tract secretions and body fluids.
Respiratory transmission may occur when large respiratory droplets or short-range aerosols from the infected host are deposited on mucous membranes or the respiratory tract of the susceptible host. Prolonged face-to-face contact, such as domestic contact, may be necessary for transmission to occur via this route. Activities involving the dispersal of dried material from wounds (e.g. shaking contaminated laundry) may also present a risk and should be avoided.
In the event of pregnancy, contamination of the foetus via the placenta can occur.
It is currently unclear whether the virus can be spread through semen, vaginal secretions, urine or faeces.
The following figure illustrates the different modes of transmission as they are currently known.
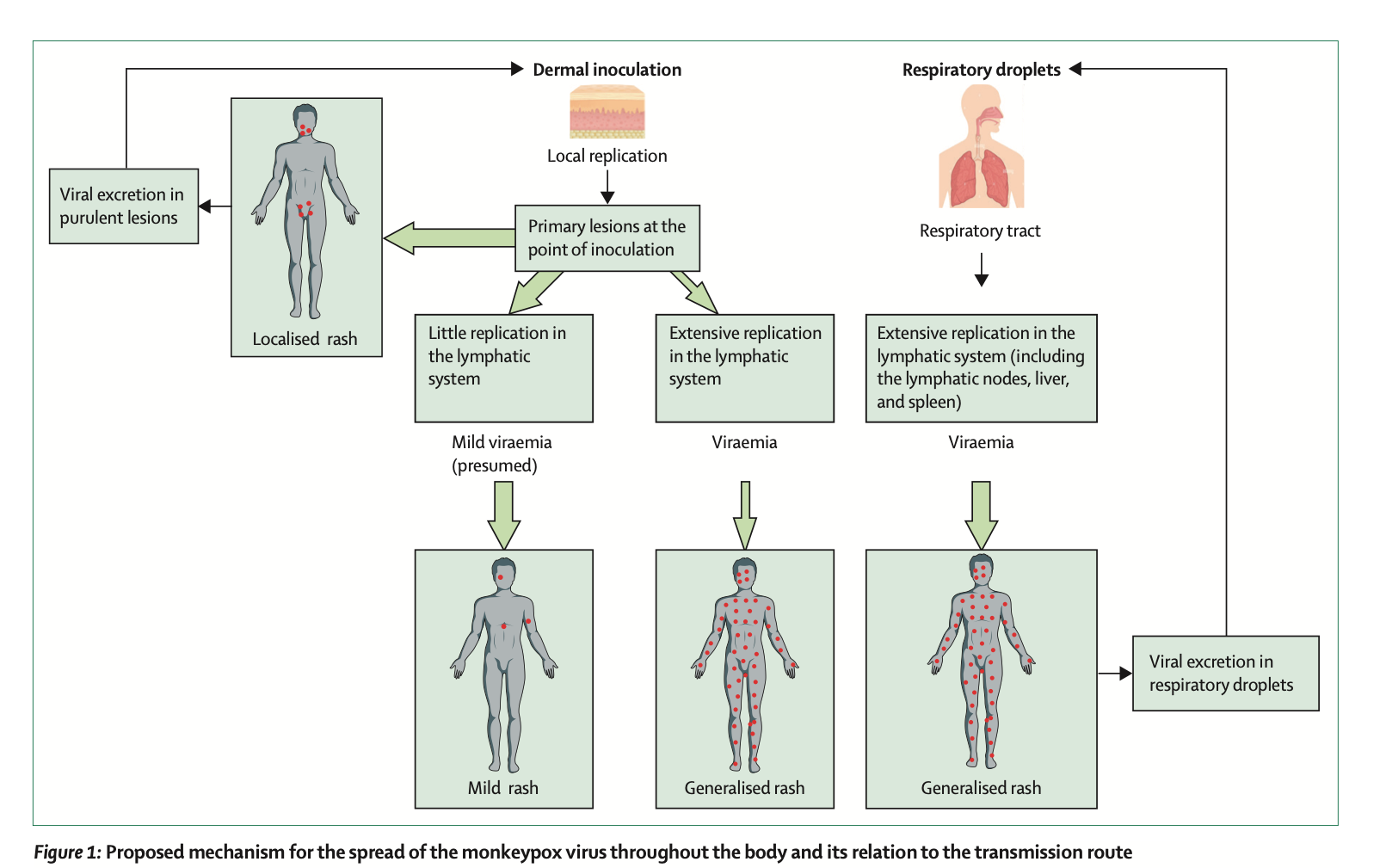
Source : https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(22)02075-X.pdf
Symptoms
Mpox causes signs and symptoms which usually begin within a week but can start between 1–21 days after exposure.
Symptoms usually start with a fever.
About one to three days after the fever begins, patients develop a rash.
It usually first appears on the face, and affects the arms, legs, hands, and feet. However, as was the case in the 2022 outbreak, the rash can also involve the genital and perianal area. The rash progresses through several stages, forming blisters, which become pustular, before crusting and falling off.
Vesicles or pustules (lesions) can be painful and itchy.
In some cases, only mild symptoms appear. The rash is discrete, with only a few or isolated vesicles or pustules.
The disease can also cause flu-like symptoms (fever, chills, headache and sore throat, muscle and back pain, etc.), or in the genital and anal area (pain, bleeding, inflammation).
An infected person may be contagious from the first symptoms until the end of the rash, i.e. until the last scabs on the skin have fallen off.
Treatment
Mpox is usually a self-limiting disease, i.e. it resolves without treatment), Most cases can remain at home with supportive care and recover within about two to four weeks.
However, children (particularly those younger than 8 years old), pregnant or breastfeeding women, or persons who are immunocompromised may be at risk of severe disease.
Pregnant/recently pregnant women with mild or uncomplicated mpox may not require hospital admission but monitoring in a health facility may be preferred. In general, those with a high risk of complications or with severe or complicated mpox should be admitted to hospital for monitoring and clinical care and to prevent transmission to others.
The decision as to whether or not to stop breastfeeding for mothers with mpox should be assessed on a case-by-case basis with a medical practitioner.
What should you do if you show symptoms or have been in contact with an infected person?
If you show symptoms of mpox, it is recommended to seek immediate medical advice and to observe the following to avoid further spreading the disease:
- You should self-isolate until the rash has healed completely.
- You should telework if possible or request sick leave depending on severity of symptoms.
- You must avoid contact with pets and immunosuppressed persons at risk of developing a severe form of mpox.
- You should abstain from sexual activity and close physical contact.
- Do not share personnel objects such as bed linen towels or crockery.
- Disinfect or wash your hands regularly.
- Disinfect bathrooms after your passage.
- If you have to leave your home, please wear a surgical mask and avoid crowded settings including public transport.
- Do not undertake any travel.
Contacts of mpox cases should self-monitor for the development of symptoms up to 21 days from the last exposure to a case. Some authorities are recommending that close contacts isolate for 21 days.
Contacts are defined as a person who has had one or more of the following exposures with a probable or confirmed case of mpox while it is infectious:
- direct skin-to-skin and skin-to-mucosal physical contact (such as touching, hugging, intimate or sexual contact),
- contact with contaminated materials such as clothing or bedding (including materials dislodged from bedding or surfaces during handling of laundry or cleaning of contaminated rooms),
- prolonged face-to-face respiratory exposure in proximity.
Vaccination
Mass vaccination is not recommended for mpox at this time, but vaccination can be considered as post-exposure prophylaxis (PEP) for contact of cases and as pre-exposure prophylaxis (PrEP) for certain high-risk groups.
Vaccines are available in France and Switzerland for specific target populations (see sources and references below) but are not widely available.
Smallpox vaccination also provides some protection against Monkeypox.
A newer vaccine that protects against smallpox and mpox is available in a few locations, for use in people who may be exposed through their occupation, under strict protocols.
Prevention
Prevention is through:
- Observing good personal hygiene.
- Washing hands well and often.
- Avoiding close contact with sick people.
- Avoiding touching objects which have been in contact with a sick person.
- Following safe sex practices, including condom use. Condom use will not prevent contracting mpox if lesions are not covered but will protect against sexually transmitted infections.
- Wearing face masks. This is particularly relevant for high-risk groups in areas were the virus is in circulation.
In areas where mpox is present in animals, additional preventive measures are:
- Avoiding contact with wild animals.
- Avoiding touching objects which have been in contact with animals.
- Avoiding eating inadequately cooked meat and other animal products of infected animals.
- Avoiding preparing or eating "bush meat" (wild game).
Sources and references - further information:
- General information (WHO)
- General mpox information - Switzerland
- Vaccination information sheet (in French)
- General mpox information - France (page automatically translated into English)